Why Medicare Coverage is Critical to Caregivers
Why Medicare Coverage is Critical to Caregivers

Why Coverage with Evidence Development (CED) Hinders Patient Access & Increases the Caregiver Burden
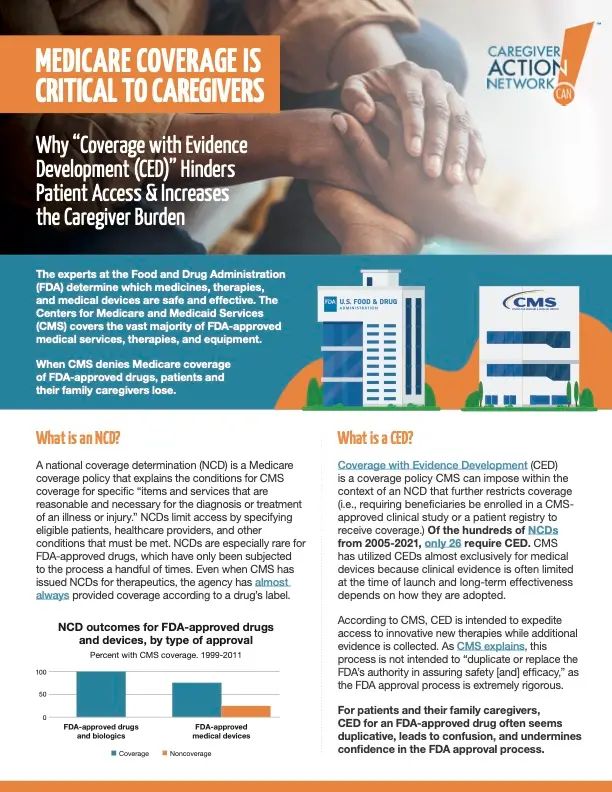
The experts at the Food and Drug Administration (FDA) determine which medicines, therapies, and medical devices are safe and effective. The Centers for Medicare and Medicaid Services (CMS) covers the vast majority of FDA-approved medical services, therapies, and equipment.
When CMS denies Medicare coverage of FDA-approved drugs, patients and their family caregivers lose.
What is an NCD?
A national coverage determination (NCD) is a Medicare coverage policy that explains the conditions for CMS coverage for specific “items and services that are reasonable and necessary for the diagnosis or treatment of an illness or injury.” NCDs limit access by specifying eligible patients, healthcare providers, and other conditions that must be met. NCDs are especially rare for FDA-approved drugs, which have only been subjected
to the process a handful of times. Even when CMS has issued NCDs for therapeutics, the agency has almost always provided coverage according to a drug’s label.
What is a CED?
Coverage with Evidence Development (CED) is a coverage policy CMS can impose within the context of an NCD that further restricts coverage (i.e., requiring beneficiaries be enrolled in a CMS- approved clinical study or a patient registry to receive coverage.) Of the hundreds of NCDs from 2005-2021, only 26 require CED. CMS has utilized CEDs almost exclusively for medical devices because clinical evidence is often limited at the time of launch and long-term effectiveness depends on how they are adopted.
According to CMS, CED is intended to expedite access to innovative new therapies while additional evidence is collected. As CMS explains, this process is not intended to “duplicate or replace the FDA’s authority in assuring safety [and] efficacy,” as the FDA approval process is extremely rigorous.
For patients and their family caergivers, CED for an FDA approved drog often seems duplicative, leads to confusion, and undermines confidence in the FDA approval process.
CED can have several unintended consequences, including:
Limiting patient access
Limiting the type of patients who may benefit from a certain type of treatment, diagnostic tool, or therapy, means that many others will not have access. Family caregivers’ top priority is to ensure that their loved ones have access to all tools and therapies they need.
Threatening R&D
The time and money required to put a drug through the FDA-approval process is significant. If CMS requires additional data—beyond ongoing reporting commitments to FDA—as a condition for coverage, research and investment incentives will be reduced.
Increasing Costs
A review of CEDs found that CMS does not directly fund the clinical research detailed in NCDs, therefore public and private funding streams are required to develop and conduct the research in question.
Extending treatment delays for patients
One expert explained that, for CED, “generally, a maximum of four years until study completion and final decision seems to distinguish successful from unsuccessful cases.”
For most disease states, timely and accurate diagnosis is critical to help ensure timely, effective treatment.
Unclear or confusing data requirements
Currently, data collection mechanisms are designed and implemented without a specific timeline for coverage reconsideration. This is exemplified by the lengthy and widely varying program duration for the three out of 26 programs with retired data collection requirements (4 to 12 years) and the long duration of the two CED programs resulting in NCD revocation (10 and 13 years) since 2005.
Increasing Health Inequities
CEDs could add to the significant health equity gaps for rural and underserved communities, and people of color. Participants in approved studies may receive better treatment than those not participating, and treatments likely will not be available in all geographical areas. A recent Avalere analysis provides a detailed look at the health equity issue.
Ethical Issues
Various stakeholders have questioned whether it is ethical to restrict access to FDA-approved therapies to patients participating in registries and clinical trials while withholding coverage for others. Patients and caregivers must weigh a lot of factors in order to determine whether a clinical study is right for them. Further, when CMS requires randomized control trials, there is a risk that patients will receive placebo.
How Can CMS Better Help Patients and Caregivers?
- Clearly articulating a pathway to coverage.
- Utilizing a fit-for-purpose data collection process that is designed to answer specific, necessary questions.
- Reducing health equity gaps by allowing flexibility for all appropriate providers to participate, even if entities have minimal data infrastructure capabilities.
- Clearly defining the time limits or stopping rules to ensure that patients aren’t waiting for decades for treatments.
Medicare coverage plays a vital role in supporting family caregivers and their loved ones. By understanding current policies and advocating for improvements, caregivers can help create a more supportive healthcare system. As policies continue to evolve, it’s crucial to maintain focus on reducing caregiver burden and ensuring access to necessary medical care and support services.