Stroke Caregiver GPS: When Your Loved One Has Had a Stroke
Stroke Caregiver GPS: When Your Loved One Has Had a Stroke
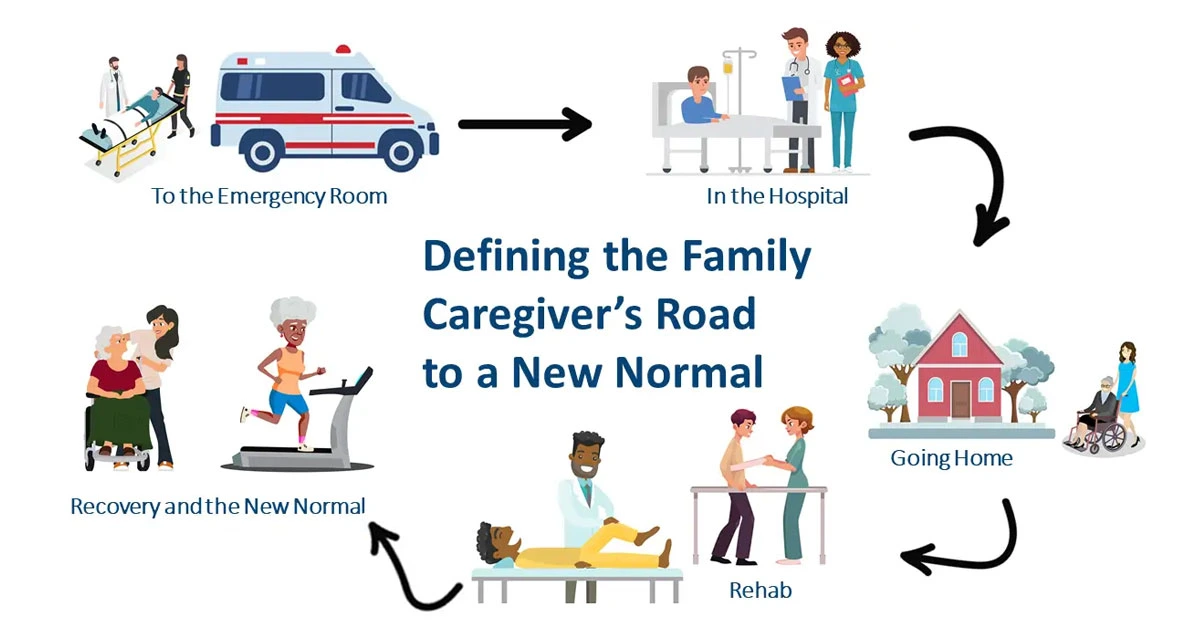
Being a caregiver for a loved one who has suffered a stroke involves significant challenges. From preparing for emergencies to managing long-term recovery, caregivers play a crucial role in ensuring their loved one’s well-being. This guide provides essential strategies and resources to support you through each stage of stroke care, from emergency room visits to home recovery.
Emergency Room Preparation for Stroke Patients
Have a Caregiver “Go” Bag Ready
Preparing a “Go” Bag can make your emergency room visit more manageable. Pack essential items such as a blanket, water, a power bar, a phone charger, and a book. Having these supplies ensures you are prepared for any situation during the emergency room visit.
Be Prepared with the Right Paperwork
Bring all necessary documents, including your loved one’s medication list, patient file, and any relevant health information like their Backpack Health info. This will help streamline the process and provide medical staff with crucial information.
Tips for Talking to Medical Staff
- Introduce Yourself: Let the medical staff know you are the family caregiver.
- Accurately Report Symptoms: Describe symptoms without making a diagnosis. For instance, say, “My Dad seems to get extremely out of breath after walking even a very short distance,” rather than, “I think my Dad has pneumonia.”
- Ask for Updates: Request updates on your loved one’s condition regularly.
- Show Appreciation: Thank the medical team for their care and assistance.
Hospital Care for Stroke Survivors
Educate Yourself
Understanding your loved one’s condition and treatment options is vital. Research their diagnosis and ask questions about their care plan. Keep track of their test results, lab work, and any procedures performed.
Talk to Your Loved One About Their Goals
Discuss your loved one’s health and recovery goals with them. Understanding their preferences and desired activities will help you align their care plan with their personal wishes.
Observe Therapy Sessions
Attend therapy sessions conducted in the hospital. Take notes on exercises and ask which ones should be continued at home to support ongoing recovery.
Plan for Discharge
Start planning for discharge early with the hospital’s social worker or case manager. Ensure that discharge plans align with your loved one’s goals and include recommendations for additional care providers such as therapists and home health aides. Ensure you have a home health care prescription if needed to cover services through Medicare.
Home Safety for Stroke Recovery
Do a Safety Evaluation of the Home
Prepare your home for your loved one’s return by addressing potential hazards. Remove throw rugs, change light bulbs, and install grab bars. Consider modifications like installing ramps or special features in the bathroom to enhance accessibility and safety.
Handle Medical Appointments
Schedule follow-up appointments and discuss any symptoms or concerns with your loved one’s healthcare providers. Determine if additional help, such as home health aides, is required and verify what outpatient care services are covered by your insurance.
Build Your Support Network
Engage with friends and family to build a support network. Seek out support groups and resources for caregivers to help manage emotional and practical challenges. For additional support, explore resources provided by Caregiver Action Network.
Stroke Rehabilitation Options
Decide on Rehab Plans
Choose a rehabilitation plan based on your loved one’s recovery goals. Options include self-managed care, nominal care, essential care, or comprehensive care. Discuss these options with healthcare providers to select the best approach for your loved one’s needs.
Keep a Journal of Your Loved One’s Progress
Track your loved one’s progress by documenting successes, challenges, and any new symptoms. Share these observations with doctors and other family members involved in the care.
Recovery and the “New Normal”
Take Care of Yourself
Prioritize self-care by setting aside time each day for yourself. Attend support group meetings, seek help when needed, and explore respite care options to manage caregiver stress effectively.
Understand the “New Normal”
Recognize that both you and your loved one will need to adapt to new circumstances. Discuss any changes in mood or behavior with the healthcare team to identify if they are related to the stroke or indicate other issues.
Watch for Warning Signs
Monitor for symptoms such as muscle spasms, severe headaches, fatigue, chest pain, difficulty breathing, and heart palpitations. Report any concerning symptoms to the doctor immediately to ensure timely intervention.